
Ask DadPad, Labour and Birth
Ask DadPad: What happens to a woman’s body after she’s given birth?
Posted on 20th April 2023
These days, many dads-to-be spend time learning about how to be a good birth partner. Antenatal education and classes play an important part in preparing both parents for birth and the early days of parenthood, although the local antenatal offer does vary depending on your location and between individual providers.
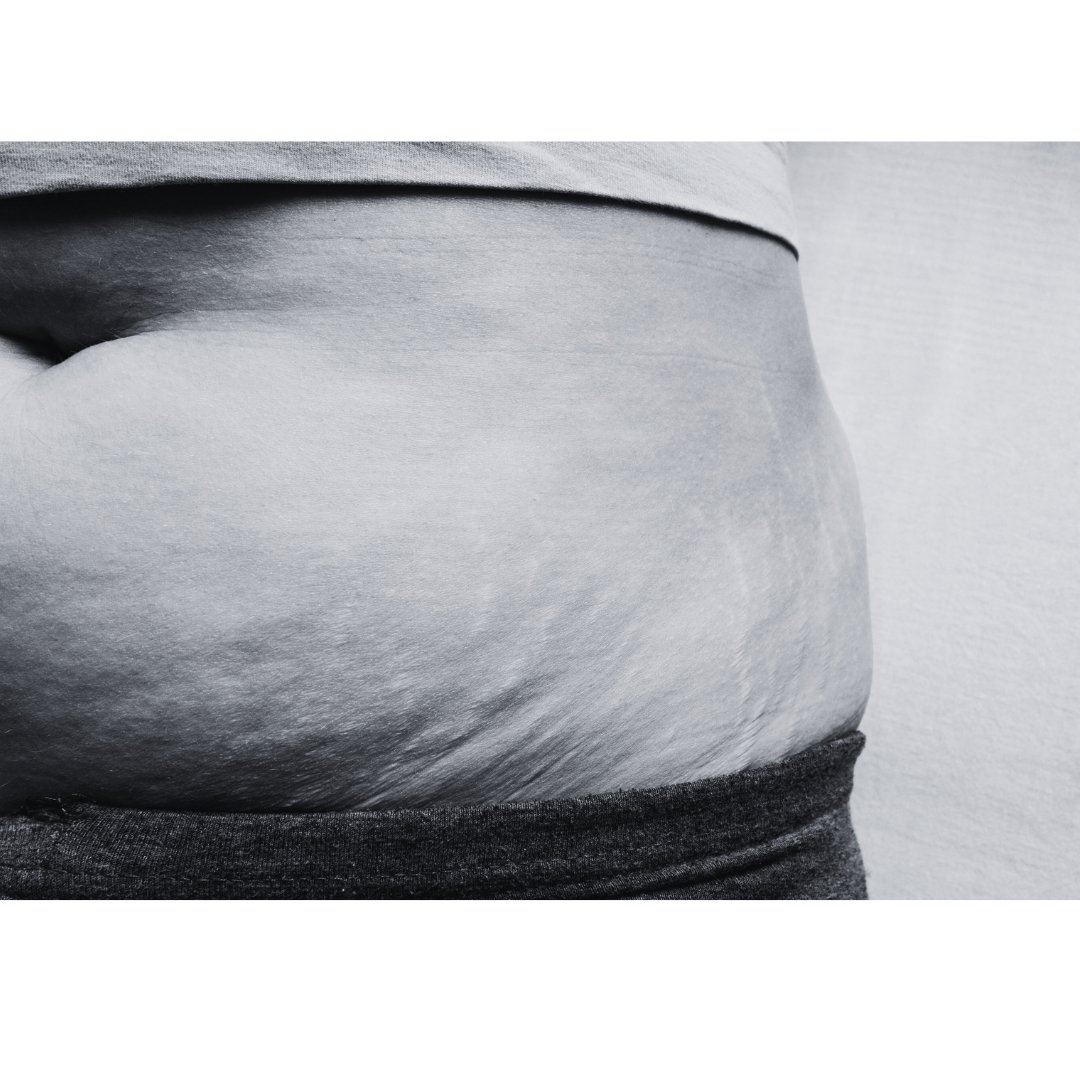
One thing that is often not shared in any detail during this antenatal education, though, is what happens immediately after the woman has given birth, and also during the initial recovery period. The realities of the post-birth (or, to give it its proper name, post-partum) body are also not often accurately represented on social and other media. Pictures of glamorous, recently-birthed women with barely a hair out of place, or those of women who are one week in with their new baby and already back in their pre-pregnancy skinny jeans really don’t help those with no experience of birth and recovery get an accurate picture of what to expect*. We’ve therefore asked Georgie – DadPad’s Project Officer, who’s also an experienced birth and postnatal doula – to craft this blog on the post-birth recovery period, with dads in mind, so you feel more ready and know the importance of the supporting role you’re going to need to perform over the coming hours, days and weeks to help your partner.
Georgie’s blog aims to help dads (and anyone else who’s interested!) better understand what happens to the human body after birth, the medical care that may be offered or needed following birth, and how the post-birth recovery might affect a woman’s physical and mental wellbeing.
* NB. And no shame to those women who are able – and want to celebrate being able – to do these things. We just think it’s important for dads-to-be to know that this isn’t necessarily going to be what their birthing partner will experience, and that that’s completely normal.
Immediately after the birth
Whilst the birth of your baby is the main event of labour, and will inevitably and understandably take up the majority of your energy and focus, it’s important to know that there is a final stage of labour, which takes place after the birth. Being aware of all that will happen immediately after the birth can help you better appreciate why the post-birth recovery often takes longer than you might think…
To make this information as easy and uncomplicated as possible, I’ve summarised the most significant parts of the immediate post-birth stage, in relation to mum’s body, as follows:
Birthing the placenta
The placenta is a unique organ that grows inside mum’s uterus (or womb) early on in pregnancy and which connects to your baby via the umbilical cord throughout pregnancy. The placenta acts as a filter between mum’s body and your baby, to pass oxygen and nutrients to baby, and to remove waste products from your baby’s blood. When your baby is born, the placenta will remain inside mum initially, and your baby will also remain connected to it via the umbilical cord (which will be cut within a few minutes of birth).
When the placenta has finished its job, it’s no longer needed and it is time for it to come out. The placenta will need contractions from mum’s body to help separate it from the wall of the uterus and to be pushed out, in the same way your baby was (unless your partner has had a Caesarean section, or C-section, in which case the placenta will be manually removed from mum through the same incision that your baby was born from). Mum can either decide to wait for the contractions to re-start on their own, or she can opt for an injection of artificial oxytocin, to encourage the process along.
As with any medical intervention, there are risks and benefits to each option, and your partner will need to think about what is right for her. She will have considered this and other potential pre-birth, birth and post-birth medical intervention options with her Midwife when they (and maybe also you?) discussed her ‘birth plan’, at an antenatal appointment in the weeks leading up o the birth. Whatever choice she makes, the Midwife or Obstetrician supporting her labour care will keep a careful eye on the process and may intermittently check that the placenta has detached by gently applying traction to (i.e. very gently pulling on) the umbilical cord.
The Midwife or Obstetrician attending to your partner will carefully check over the placenta to ensure that it is healthy and has come away in one piece. New mums can become very unwell if part of the placenta, or any other waste parts of the pregnancy, are left behind inside them, and may need to undergo a manual removal process if the placenta hasn’t come out in one piece.
If you want to see the placenta for yourself – after all, it’s been doing amazing work, helping your baby to grow for the past 9 months, and it’s a pretty phenomenal structure – ask the Midwife or Obstetrician to show you it as they check it over. You might be surprised at how big it is! You and your partner can also choose to take the placenta home, if that’s what mum wishes to do; otherwise it will be medically disposed of at the hospital.
[If you or your partner want to investigate some options of what you can do with your placenta – including donating it and/or the cord blood cells for medical purposes – have a look at this article. Before viewing, though, do be aware that there are lots of photos here – albeit all in black and white – of both placentas and post-birthing mums.]
After the placenta has been birthed, the contractions will continue intermittently for a few hours or days, especially when mum is cuddling or feeding the baby. These contractions are often called ‘after-pains’ and their intensity tends to vary depending on how many times mum has given birth before; women generally report that their after-pains feel more intense and continue for longer the more times that they have given birth.

Post-birth bleeding
It is perfectly normal for mum to bleed after your baby has been born. The Midwife or Obstetrician caring for her will keep an eye on the amount of post-birth bleeding, and may offer further interventions to help manage the bleeding, if needed and depending on how much blood they have calculated has been lost.
Once baby has been born, the placenta is out and mum is ready to get up, she will need to have maternity pads and maybe also disposable underwear – it would be really useful to know where these items are in her maternity bag, in case she asks you to get them for her. The first blood after the birth will be red, heavy and may contain some clots. For this reason, her maternity pads will need changing regularly, for both comfort and hygiene reasons, and again this is something that she might need your help with, at least to start off with.
This post-partum bleeding (sometimes called lochia) continues for around six weeks after birth, but will become increasingly less-blood-like, with a lighter flow, as the weeks go on. Do reassure mum that it’s ok to ask a medical professional – such as their Midwife, Health Visitor or GP – to have a look at any heavily-soaked pads, clots or discharge colour or smell that concerns her. It might sound a bit icky to us, but these professionals are used to looking at such items and will always prefer to check and reassure, than risk mum getting ill for fear of sharing something relatively personal.
It’s also important to be aware that many women find that their post-partum bleeding can feel like it suddenly floods their pad, gets worse or returns after stopping if they get up from a reclining position too quickly, or overdo things during the first 6-8 weeks of recovery.
If you or baby’s mum want to find out more about post-partum bleeding, the NCT have written a really helpful article which you can read here.

Post-birth checks
Both baby and mum will be offered post-birth checks by the team around your family.
For mum, the post-birth check might feel quite invasive. General observations will usually be taking place in the background, to ensure that mum is recovering ok, until they are ready for anything else. Part of the ‘cleaning up’ process will also involve being offered a physical examination to assess any potential damage to her body. If your partner does consent to this examination, she’ll need support to get into a comfortable position and/or have help to hold baby whilst it happens, as it’s likely that she’ll be feeling tired and tender by this point.
The person conducting the post-birth check should talk through with your partner what they are going to do and what they are doing, offer additional pain relief before starting, and stopping whenever mum requests that they do. The post-birth physical examination usually starts with an external examination of mum’s body, under good lighting, and will then usually progress to an internal examination, to check – as gently as possible – for any internal damage. The Midwife or Obstetrician performing the examination will talk through with mum what they find, and what they recommend to help heal or repair any damage.
It is common for birthing women to have some grazing or minor tearing from giving birth, which usually recovers on its own. However, some tearing may benefit from being repaired with stitches, which will be inserted either in the labour room or in theatre.
During any repair – and after it has been completed – mum may need further pain relief; she might also require referral to a specialist Urogynaecology and/or Pelvic Physiotherapy Service for further treatment and support as she continues to recover in the coming months.
If your partner wants to find out more about recovering from tearing during birth, you could share with her this NHS video which covers that very topic.

Getting moving again
Recovering from labour can feel like recovering from an ultra-marathon! Very quickly after your baby has been born, you may find that your partner becomes quite shaky and feels very weak. She will need something to eat and drink to help with any post-labour energy crash – the Midwife who’s supported your partner’s labour can help you with this, by bringing her tea and toast, if you are low on snacks from your hospital bags at this point.
It’s likely that baby’s mum will need help to move positions in bed, especially if she’s had an epidural, has had stitches and/or been in one position in labour for a long time.
Moving about will get easier over the coming days; however, as bruising begins to develop and as stitches start the process of healing, your partner’s mobility and pain levels may vary. If she had a C-section, then she will need significant support, as she will also be recovering from abdominal surgery, as well as having given birth, and so will not have much core strength to begin with.

Using the bathroom
When she’s stable enough after the birth, and feels ready, she will want to use the bathroom and freshen herself up. It’s likely that she’ll need someone to help her with this, because she may not have full sensation again yet and/or might still be feeling very weak.
One of the most important things that Midwives will be wanting to check on during the initial stages of post-birth recovery is that your partner is regaining the use of her bladder and bowels again. Mum will therefore be regularly asked by her Midwives about her bladder and bowel movements in the early days after giving birth. Whilst she may feel embarrassed about discussing her weeing and pooing, and may also be worried about how to recover, it is normal for things to take time to get going again. Midwives also have different tools and techniques which can help things along, if needed.
All women – but especially those who have had stitches to repair tears – will experience discomfort when urinating in the early days after birth. Swelling and bruising can temporarily alter her sensations in relation to holding or releasing her wee, and any grazes or tears can really sting when they come into contact with urine.
Many new mums find it easiest to wee into fresh water, as the water helps to dilute their urine, taking away the initial sting and also helping to keep the area clean, without the need for lots of wiping. You could therefore support your partner, if she is finding it painful to relax enough to wee and to deal with the pain, by suggesting that she wee either into a running shower or whilst sitting in a shallow bath, or that she pours fresh, warm water from a jug or sports bottle onto herself as she urinates.
If she’s struggling to have a poo after giving birth, you can again offer support by ensuring that she has something to hand in the toilet to help raise her knees up a bit so that she is in more of a squatting position; toddler toilet steps are a great idea for this, or any other low-ish foot stool that you have in the house – or maybe even a box or a pile of books?! She might also want to hold a clean maternity pad over her vulva and perineum (the area of skin between the vaginal opening and anus) whilst she poos. By getting into a more optimal position, and by applying positive pressure to the areas that feel tender, sore and open, mum will be able to give herself the best chance of being able to relax the muscles that control her bowels and breathe out those initial bowel movements, avoiding too much bearing down or straining.
There’s also some helpful information to new mums on going to the toilet after birth on this NHS webpage.
As soon as mum regains some feeling and control, she will be encouraged to start exercising her pelvic floor again, with some daily exercises. These exercises will further help mum’s bladder and bowel control, and help her to gauge her body’s recovery from pregnancy, birth and labour over the coming months.

The early days
The postnatal ward
Not every woman needs to stay on the postnatal ward after giving birth and, if the pregnancy has been low risk with the labour and birth straightforward, it is common for new mums to be able to go home around six to 24 hours after your baby has been born (if you aren’t already at home, following a home birth). If this is the case, the Midwife looking after your partner will discuss this option with you, to check how you all feel about this, and also outline the plan on how any postnatal care that mum or baby might need will be provided in the community.
Not everyone feels ready to go home so soon after giving birth, though, and it’s OK to request to spend some time on the postnatal ward first. One of the benefits of doing this is having access to further medical support and a range of pain relief.
For those families where the pregnancy or birth has been a bit more complicated, such as if your baby was delivered via a C-section, or where mum or baby need a little more care following the birth, it’s common for the professionals looking after your new family to recommend that mum and baby spend some time recovering on the postnatal ward before going home. If this additional care is deemed necessary for those who’ve given birth at home, or in a stand-alone Midwifery-led Unit, this may include a discussion on how to safely transfer mum and baby to the hospital by ambulance; otherwise, transferring mum and baby to the postnatal ward usually just involves a short trolley or wheelchair ride from the birthing room, once mum has had the chance to initially recover from giving birth, get checked over and freshen up.
If you are able to stay on the postnatal ward with your new family (which isn’t always the case in every hospital, to do find out about this beforehand, as part of your antenatal preparations), don’t forget that you are best placed to notice anything out of the ordinary, as you know your partner best.
At whatever point that your partner feels well enough to go home after giving birth, don’t forget to ask before you leave about additional pain relief and for information on things to look out for.
Returning home
Once you get home, you’ll hopefully be able to support each other in the care of your new baby, and in mum’s recovery from the birth. As her closest companion, though, you have another important role in these early days, which is to be on the lookout for any of the following things happening to your partner:
- feeling significantly weak or faint;
- a high temperature or heart rate;
- breathlessness or chest pain;
- pain, swelling, tenderness, warmth or aching in her legs;
- significant bruising;
- bleeding which soaks maternity pads quicker than expected, or the passing of large clots;
- pain which is not well-controlled by pain relief;
- stitches which come undone, or which are too tight;
- sticky, oozing or smelly wound sites;
- difficulties passing urine or faeces;
- continued poor pelvic sensation or pressure, heaviness or pain in or around the vagina;
- breastfeeding challenges; and/or
- significant changes in her behaviour, or a decline in her mental wellbeing.
If you notice any of these, do make sure that you encourage your partner to discuss them with the healthcare team supporting your family at the earliest opportunity (or seek help directly yourself, if mum isn’t able to do so). Your Postnatal Ward or Community Midwives will be available to support and advise you all throughout mum’s early postnatal recovery, for around 28 days after your baby’s birth. They can provide physical and emotional support, check and redress any healing wounds, and give further advice or make relevant onward referrals to other specialist services, if required. Your GP or Health Visitor should also be able to provide additional support, monitoring, treatment or onward referrals if you are not able to see a Midwife quickly, or if your partner has already been discharged from Midwifery care.
If mum suffers from a really serious bleed after birth, you should call 999 immediately. As set out on the NHS website, sudden heavy bleeding, together with feeling faint, dizzy or having a pounding heart could mean that mum is experiencing what’s called a post-partum haemorrhage and she will need emergency treatment ASAP.
Aiding mum’s recovery
Regardless of how smooth labour and birth went, every woman will need to take it easy in the early days. Resting is important for postnatal recovery and general wellbeing, as being on your feet for prolonged periods, overdoing things physically and sitting directly on wound sites for too long can result in ongoing discomfort and delay the recovery process overall.
When new mums overdo things, it can also have a negative impact on how they feel about themselves and their body, especially if they were a previously active or independent person. Their body may look, feel or behave from how it was before pregnancy and giving birth. This can have a knock-on effect on their relationship with you, so it is therefore important for you to support your partner’s recovery and to be patient with the process.
The best way to do this is to make sure that you’re ready and prepared to be as hands-on with your new baby as possible. You can find out more on how best to do this via your DadPad and/or the DadPad app (if available in your area). We’ve also got some other blog posts which might help you, including one on how to care for your baby and another on how to support mum with breastfeeding.

References and further reading:
Robertson, Jo (2019) 16 Remarkable things to do with your placenta via lcrazebirthphotography.co.uk [online]
NCT (2018) Your post-pregnancy body questions answered. [online]
NCT (2021) Bleeding after birth: 10 things you need to know. [online]
NHS (2021) Your body after the birth. [online]
NHS (2022) Early days. [online]

