
Ask DadPad, Infant Feeding, Parenting Advice
Ask DadPad: Breastfeeding – the myths…
Posted on 21st August 2020
We’re back with another blog post to help dads become the best breastfeeding supporter to their partner that they can. After having already looked at colostrum and some top tips on supporting mum, this time we’ve asked Georgie to consider some of the most common myths and perceptions about breastfeeding that you might come across.
Having family and friends to support you is an essential part of raising a baby. However, their advice and experiences aren’t always helpful when trying to make your own parenting decisions, such as how to feed your baby. This is a personal choice that you and your partner should discuss together before your baby is born. It’s a good idea to do your research on infant feeding choices, including where to find help locally in case you need it after your baby has arrived. Remember that your family’s pregnancy, birth and early parenthood experiences will be unique to you and your partner, so don’t make decisions about how to feed your baby based solely upon what someone else believes.
In this blog, we’re going to look at eight of the most common breastfeeding myths that you might hear during your new baby journey. For each, we’re going to consider where they might have come from, and whether or not they’re true. Hopefully, having this information to hand will help you and your partner if you hear them.
“If breastfeeding doesn’t come naturally from the start, there’s no point in trying to make it work.”
Many people believe that breastfeeding should just come naturally to mum; after all, they have all the equipment that they need to do it, right?! Wrong. Breastfeeding is actually a learnt skill – a bit like learning to ride a bike – and so it is only to be expected that there will be a period of learning, and a few wobbles along the way. On average, it take around six weeks for a mum and baby to master breastfeeding together, and feeling confident about doing it outside of your home may take even longer. With the right support and encouragement, though, most breastfeeding challenges can be overcome.
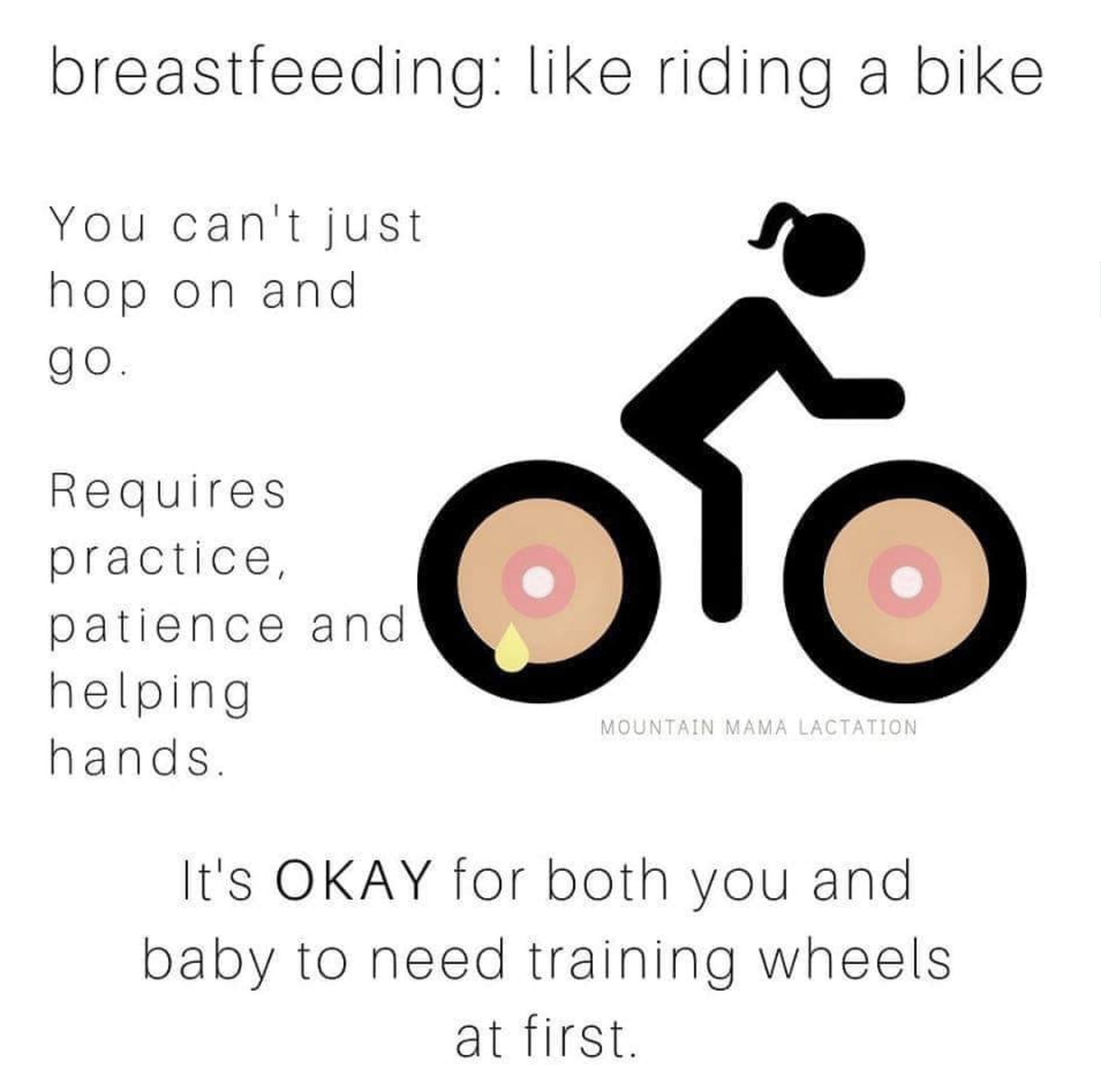
We love this image, shared on Facebook by various pages, including the Boulder City Breastfeeding Support Group and Milky Mommas Inc.
“I never made any milk and my baby was starving.”
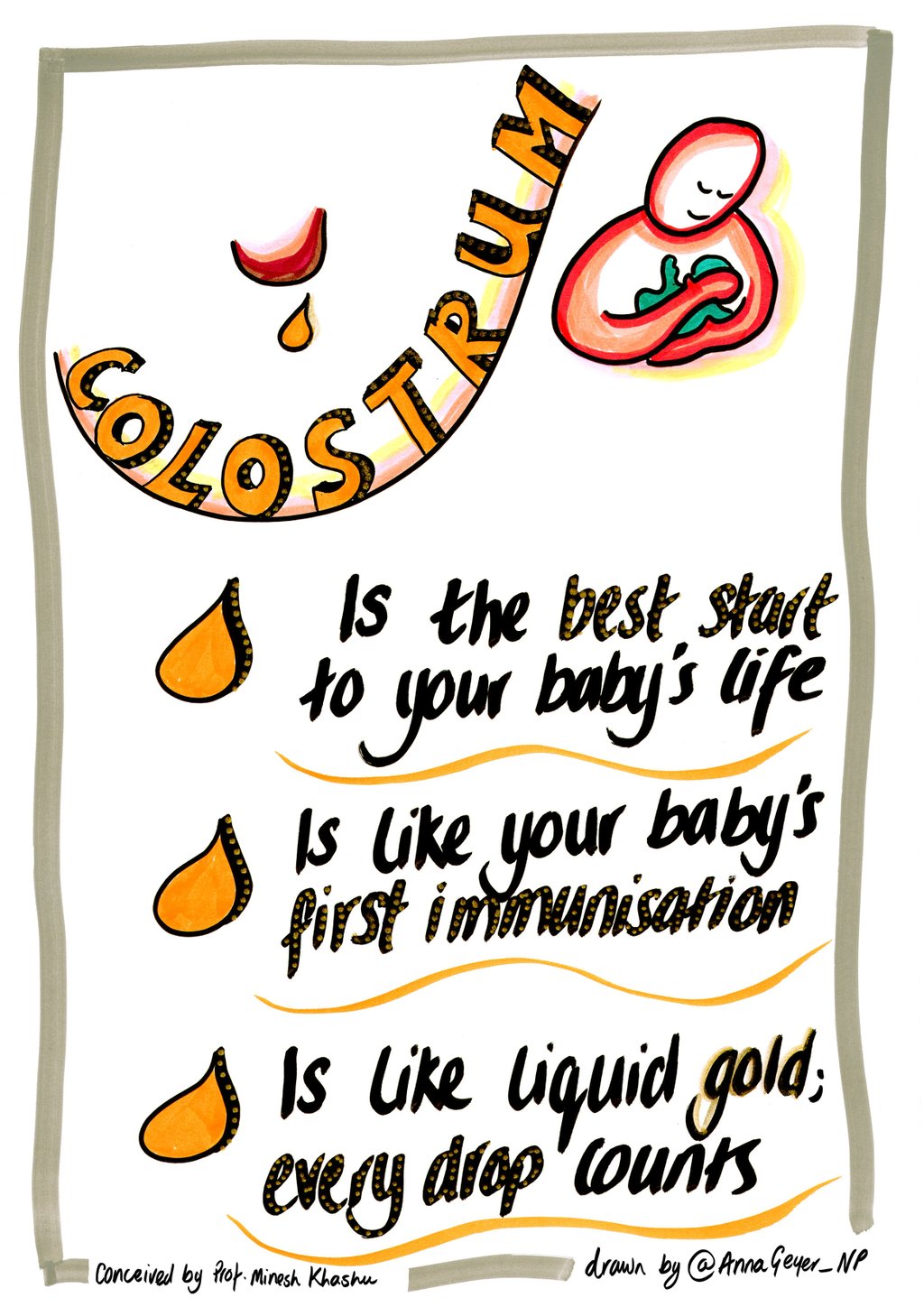
This is a common reason why mums give up breastfeeding before they are ready, and it is built upon the assumption that human milk should look exactly like dairy milk, and be produced in large amounts. During pregnancy, your partner will begin to produce colostrum from her breasts. Colostrum is a thick, sticky, nutrient-rich substance and will be your baby’s first milk, containing everything that your baby needs in the early days after birth. Some women notice leaking and some don’t, but this has no reflection on whether or not she will be able to successfully breastfeed when baby arrives.
When your partner gives birth to your baby, chemical signals (called hormones) trigger the brain to start the process of maturing the colostrum into a full milk supply. As the early days pass, responsive feeding (i.e. feeding your baby whenever he requires to be fed) will prime the breasts to make a full milk supply, and you will start to see that the colostrum becomes thinner, changes colour, and becomes more recognisable as milk. This process – known as her milk coming in – can take between 3 and 14 days, following birth, and can be affected by the kind of birth that mum experienced. If mum’s milk is taking a while to come in, it is important to seek specialist support to make a feeding plan.
Most initial feeding difficulties – which some mums might interpret as a sign that they are not able to produce any/enough milk – are quickly and easily overcome by chatting with your midwife or health visitor about your concerns. It might be something as simple as an incorrect latch, the need for an altered feeding position, or – occasionally – that baby has a tongue-tie. However, almost all are easily remedied and, once this is done and baby is able to latch and suck more effectively, then mum’s body will produce more milk and feeding will progress positively.
Some mums also worry that their baby isn’t getting enough milk or that their milk has dried up when baby has a day or two of what feels like continuous feeding. Although this might feel like baby isn’t getting what they need from mum’s breasts, it’s more likely that baby is having a growth spurt and just needs to feed more for this short period of time. He’ll soon settle back down to normal feeding patterns again.
You will know if your baby is feeding well as they will be gaining weight and you are changing plenty of wet and dirty nappies.
For only a very small minority of mums will breastfeeding not be possible, usually due to an existing medical condition.
“Breastfeeding is painful.”
Whilst some mums do experience pain in the early days of breastfeeding, it should not be something that they have to endure over the longer term. Painful nipples or breasts throughout – or in between – feeds is a sign that something isn’t quite right with the baby’s latch or feeding position. It is important that you let your midwife or health visitor know about this as soon as possible, so that they can offer baby’s mum additional help, or refer her to the right specialist support. Most of the time, just having someone observe a feed and offer some pointers will be enough to put an end to painful breastfeeding, but – occasionally – more specialist assistance may be needed.
“My boobs are too big/too small.”
Breast size is another common reason for some mums lacking confidence in being able to breastfeed their baby. The reality is that there’s no difference in the milk-making capabilities of big or small breasts; it’s all about how regularly those milk-making hormones are being triggered, either by breastfeeding or expressing once baby is born.
Breasts come in all shapes and sizes and what works for one mum and baby might not work for another. By supporting your partner to explore different feeding positions that work for her body, you will also be supporting your baby to feed well, too.
Occasionally, mum and baby might struggle to feed due to mum’s breasts either being engorged (which means they’ve become ‘over-full’ and, as a result, feel quite hard and possibly painful) or producing too much milk. In both instances, baby can find it difficult to successfully latch and feed. It’s worth (as always) speaking with your health visitor or local breastfeeding counsellor about this if it happens to your partner, as they will be able to have a look at the situation and give you both advice on how to overcome it. There’s also some helpful information on this on the NHS Breastfeeding webpages (link below).
“A baby needs to be fed to a routine.”
This breastfeeding myth originates from outdated practice. Years ago, the professional advice (which your mum or mum-in-law might have received) was to feed your baby at scheduled intervals, to prevent baby from under- or overfeeding, and to give mum’s body the opportunity to replenish her milk supply. The latest evidence, though, shows us that this is simply not the case, and feeding in a scheduled way can actually cause issues with mum’s milk supply and baby’s physical and emotional wellbeing; to ensure that baby feels secure, he needs to be fed whenever he ‘asks’ to be fed. Feeding responsively (sometimes also called ‘feeding on demand’), even it is has only been a few minutes since the last feed, is the key to growing a happy, healthy and secure baby.

“Babies who are breastfed aren’t as content.”
Breastmilk is perfectly formulated for your baby’s needs; it is always ready to serve and is easy to digest, making it the ultimate convenience food. The nutritional composition of breastmilk is complex, due to the fact that it is live and contains antibodies (a protein that helps the body to fight diseases), in addition to all the vitamins, minerals and fats that your baby needs in order to thrive.
A baby’s gut can digest breastmilk very easily, so there is very little waste product, which results in different poos to that of a baby who is being fed formula. Some people think that babies fed breastmilk will wake for feeds more frequently than formula-fed babies – you might, for example, be advised by a friend or family member to give baby a bottle of formula before bed, so that you can get more sleep at night. However, frequent waking is normal behaviour for babies and is an important protective response to reduce the risk of Sudden Infant Death Syndrome (SIDS, also known as ‘cot death’).
“Breastfeeding is embarrassing.”
Some people feel awkward when it comes to breastfeeding, because they struggle to separate the biological function of breasts from how breasts have been sexualised in society. This can make some mums feel hesitant about feeding around friends and family, and in public. Breastfeeding in public is protected by law in the UK and these days it is rare to receive negative comments about doing it.
The international sign for breastfeeding is often used to indicate a location where mums can go to feed.
Mums can also buy special breastfeeding clothes, use clothing ‘hacks’ (like the one-top-up, one-top-down method) or covers to minimise the extent to which they are, or feel, exposed, but what they really need is to build confidence. Helping your partner find a spot to feed where she feels comfortable, reassuring them that what they are doing is natural, and keeping them company is the key to overcoming feelings of nervousness or embarrassment. Local breastfeeding support groups are great places to practice breastfeeding in public in a supportive environment, as well as accessing parent-to-parent support.
“If I breastfeed, dad won’t get the chance to bond with our baby.”
We looked at this final common myth in our previous breastfeeding blog post and, as we considered there, this just isn’t true. It’s important to recognise that there are lots and lots of different ways – all of which can be just as much ‘fun’ and as rewarding – for you, as a new dad, to get to know your new baby. Yes, baby needs mum in order to be able to feed, and they will experience lots of special one-to-one times when they do this, but that doesn’t mean that you won’t be able to create similar experiences with your baby, right from the start. We’ve considered some of the ways that dad and baby can bond in our baby bonding blog post.
Where to go for further support
Obviously, you will hopefully be one of mum’s “first choice” supporters as she and your baby get to grips with this new skill. Not only does this mean being there to offer hands-on practical, as well as emotional, support whenever she needs it – but also to seek out further information and assistance, as needed. Our next blog post will include detail on and links to further reading on all sorts of ‘how-it-works’ information, which will hopefully help you in this respect.
In terms of seeking further help, though, key ideas include:
- a helpful, supportive and experienced mum-friend or family member – someone that your partner trusts, and who will support her in her feeding choices, is important!
- your midwife or health visitor – it’s really useful if you can be present when mum asks for and receives advice from this person, as this will enable you to be up-to-speed when it comes to carrying on supporting mum when it’s just the two of you with baby
- a local breastfeeding support group – most towns now have regular breastfeeding support groups/meet-ups, where mum can go with baby and get support, advice and assistance from trained breastfeeding supporters, as well as chatting with other mums about all-things-baby. Getting to these groups for the first time can be a bit of an ordeal (it might be the first time that mum has left the house with baby), so she may need some gentle encouragement, but it’s a great chance to feel a bit more ‘normal’ again, and finding out that other mums are experiencing the same difficulties as you can really help. Always ring first, though, to check that the group is still running as advertised/that the meeting is on that week/etc – the last thing that a new mum needs is to go through the effort of getting herself and baby ready for a trip out, only to find that it’s been a wasted journey. It’s also worth checking in advance to see if you and/or any older children that you have will also be welcome to attend, as different groups will have different arrangements. To find out what’s available in your area:
- if you’re in an area of the country where the DadPad app is available, have a look within your Local Services section to see if any breastfeeding support groups/information has been listed
- ask your midwife/health visitor for a list – they often provide these anyway (e.g. within your ‘Red Book’)
- go to the Association of Breastfeeding Mothers’ (ABM) webpage and type your location into their Find a local support group search page
- go to the La Leche League GB (LLLGB) webpage and type your postcode into their Find an LLLGB support group search page
- go to the National Childbirth Trust (NCT) webpage and visit their How to find breastfeeding support in your area when you need it webpage
- try Googling ‘breastfeeding’ alongside the name of your county
- you could also try your local council’s Family Information Service (FIS) – visit the Find Your FIS website to find the FIS website for your locality
- online and phone sources of breastfeeding support – there are a number of organisations offering support to breastfeeding families, either online and/or via phone support services. You can find out more via:
- your midwife/health visitor, who may also provide you with a list of local support phone numbers
- the NHS Start4Life Breastfeeding help and support webpage, which includes information on the ‘Breastfeeding Friend’ from Start4Life, available on Amazon Alexa, Google Home and Assistant and Facebook Messenger
- the Breastfeeding Network’s National Breastfeeding Helpline webpage, which offers both a phone helpline and a web-based live chat
- the LLLGB Get support webpage
- the ABM’s Breastfeeding Helpline information page
- The Pregnancy and Baby section of the NHS website also has great information on breastfeeding and common breastfeeding problems (including breast engorgement and producing too much milk).

